Our teacher, our mentor, our doctoral advisor: Professor Michael Beck, whom we still called our "chief" with great pleasure, has gone. He leaves behind a big blank.

Our teacher, our mentor, our doctoral advisor: Professor Michael Beck, whom we still called our "chief" with great pleasure, has gone. He leaves behind a big blank.
Michael Beck worked until his retirement at the University Medical Center Mainz, where he had gained worldwide renown for the University Medical Center and the city of Mainz as founder and director of the Villa Metabolica. In recent years, he contributed to the establishment of our clinical research institute SphinCS.
From the beginning of his professional career he dedicated himself to the care of seriously ill people, mostly children, with genetic diseases, especially lysosomal diseases. With great humanity and heart and soul, he accompanied affected families on their difficult journey, gave them hope, confidence and vigorously advocated offering possible treatment studies to our patients here. In addition, he was very enthusiastically involved in science, research and teaching. He shared his knowledge with us, accompanied us on our professional and private way, encouraged and supported us as a doctoral supervisor, chief and friend.
Dear Michael, we thank you for your tireless efforts and trust. We will miss you very much.

Clinical research for lysosomal diseases is fortunately receiving more and more attention. We would like to help you stay up to date and inform you accordingly about studies currently taking place.
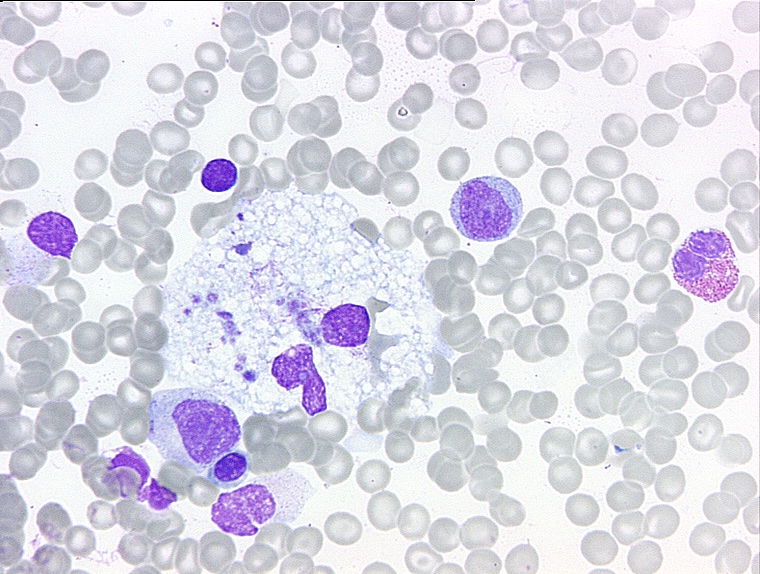
An overview of the current therapy concepts with gene therapy, haematopoietic stem cell transplantation (bone marrow transplantation), enzyme replacement therapy, substrate reduction therapy and chaperone therapy is scientifically presented in the article "Precision Medicine for Lysosomal Disorders" (Jul 26 2020). Furthermore, we have tried to illustrate the topic of therapy concepts for lysosomal diseases in a comic.

Mucopolysaccharidosis type IX (MPS IX) has been named a disease in which the enzyme hyaluronidase is deficient, and that is clinically characterized by mild short stature and notable periarticular soft tissue masses, but without neurological or visceral involvement. After the first description by Natowicz and co-authors in 1996 further cases of one family have been described who showed clinical signs of a juvenile arthritis.
Lysosomal Storage Disorders (LSDs) are a group of more than 50 rare hereditary metabolic diseases. The diseases are characterized by an abnormal accumulation of various toxic substances in the body cells as a result of enzyme defects.
Lysosomal storage diseases affect the lysosome, a structure in the cells that breaks down substances such as proteins, carbohydrates and old cell parts so that the body can recycle them. As a result, various parts of the body may be affected, including the skeleton, brain, skin, heart and central nervous system. New lysosomal storage diseases continue to be identified.